1-Month-Old
Nobody learns faster than a baby! During month two, your little one's brain is like a sponge. They've had a month to get used to life outside the womb and nailed eating, sleeping, and pooping. Now it's time to learn new things!
Your baby has been busy growing since and will typically gain around two pounds in the first two months since birth. According to the WHO growth charts, the average weight for a baby boy and girl differs slightly, at 5.6kg (12lbs 5oz) and 5.1kg (11lbs 4oz), respectively. They will have grown in height since last month, too, and boys should now be around 58cm (1ft 10.8in) tall, and girls, a little shorter at approximately 57cm (1ft 10.4in).
Don't be concerned if the soft spots on top of your little one's head are still flattened; this is entirely normal. Towards the end of this month the area should start to close and their heads feel firmer to the touch.
Speaking of heads, your baby's head grows by around half an inch every month! At this point, their head is likely to look disproportionately bigger than the rest of their body as it's growing much faster. Don't worry; their body will soon catch up! As they use their arms and legs to kick around more often and with more purpose, you'll probably notice their muscles develop and limbs change shape, and they'll start looking longer in size.
Babies' digestive system development in the second month postpartum is essential to their overall growth and well-being. During this time babies adapt to life outside the womb and become more interactive and responsive. Their digestive system matures, allowing them to process and absorb nutrients from breast milk or formula more efficiently. During this development, they may experience common issues such as colic, reflux, and gas.
At this point your baby will begin tracking people and things with their eyes, recognising familiar faces and voices, and even get fussy when they're bored and aren't engaged with or doing anything stimulating.
As they focus on things they'll also begin looking at toys and other objects and concentrate on them for several seconds. They'll also be intrigued by new faces if you have guests around who they haven't encountered before, but cut them some slack; they've still got a good few years to learn that it's rude to stare! Here’s some more information on understanding your baby’s visual development.
Hearing is one of the most well-developed senses in newborns and by the second month babies become even more responsive to sounds. They can recognise familiar voices and may turn their head towards the source of a sound. Talking and singing to your baby, playing soft music, and introducing them to different sounds and noises can stimulate their hearing development.
To aid in your baby's overall sensory development there are various activities you can engage in during the second month. You can provide colourful and visually stimulating sensory toys, mobiles, or picture books with high-contrast patterns for visual development. For hearing, you can play soft music or nursery rhymes, read aloud to them, or use toys that produce gentle sounds.
Engaging in these activities and providing a rich sensory environment can help stimulate your baby's sensory development and provide them with valuable learning experiences. It's important to remember that each baby develops at their own pace, so allow them to explore and discover the world at their own speed while providing a safe and nurturing environment.
With your little one beginning to take everything around them in and learning about new sounds and sights, now is the perfect time to start taking them out and about throughout the day on walks and car rides if you haven't been already. There are many ways to stimulate your baby in the home, but nothing compares to the big, bright outdoors!
Top tip: keep them occupied with stimulating toys that introduce them to different colours, noises, textures and feels.
Your baby will become more expressive in their emotions throughout the second month, so it should start getting easier to recognise the different cries that your baby has. They might begin to make different crying sounds depending on whether they're hungry, tired, in pain, or uncomfortable. You might also find that the time they spend crying each day is less than during the first month and they're vocalising in other ways.
While crying is still their primary method of communication, they may start showing other signs of expressing emotions. In month two some babies will smile in response to your voice or touch, signalling pleasure and contentment.
Don't be alarmed if your baby is making more cooing, gargling and screaming sounds instead of crying. These are all part of their language skills and help prepare their vocal cords for the big day when they say their first words (don't worry, you've got a while before they start answering back!).
While your little one is still too young to fully comprehend the concept of social interaction at two months, they will soon begin to show signs of social awareness. Your baby may turn their head towards familiar voices, indicating recognition and interest. They may also be curious about their surroundings and become more responsive to their environment. Encourage their social development by engaging in gentle and stimulating interactions, talking, singing, or using soft toys.
This month will show a noticeable jump in your baby's ability to express different emotions but that doesn't mean they can control them independently. During the second month your baby's ability to self-soothe is still limited. They are still firmly in the 'Fourth Trimester' and rely on you for comfort and reassurance. Gentle rocking and soft singing can help soothe your baby when upset or overstimulated. Establishing a consistent soothing routine can promote a sense of security and emotional well-being.
At around the two-month mark you will likely notice that your little one is losing the grip reflex they had as a newborn. If you've got long hair, you've probably had a lot of painful moments thanks to this reflex, and you will be glad to see the back of it!
Without this reflex they won't always grip your hand or other objects in the same way, but it will become more of a meaningful action where they grasp onto things and loosen their grip on purpose. This means they might start showing signs of holding onto things purposefully such as grabbing a toy or rattle they like and want to have! These items might look huge in your baby's tiny hands, but they're stronger than they look and can hold on for up to 30 seconds.
Developing their gross motor skills enables your little one to engage in activities that enhance their coordination, balance, and major muscle groups. These gross motor skills will help your baby develop the most basic movements as they grow, including sitting, crawling, walking, running, jumping, and climbing (although you might wish they never learnt how to climb!).
Whilst lying on their back you'll also spot that they have more control over their arm and leg movements, which become smoother and done with more purpose, looking much less erratic. They might start to wave their arms and legs when excited and begin to squirm around when they want something.
As part of this babies tend to lose what's known as the Moro Reflex at around six weeks. This reflex is the reason behind what's often called the 'newborn scrunch'. It's part of the startle reflex that babies are born with and it means that as you lift your little one up, they scrunch their arms and legs back in towards their body, leaving them looking like a scrunched-up ball of cuteness!
Does your little one look like they're trying to ride a bike? You'll get used to this movement as they grow and there's a reason it's often referred to as 'pedalling', as it looks like they're trying to ride a bike with pedals.
One of the earliest milestones people remember regarding gross motor skills is when their baby held their head up unsupported for the first time. During this month don't worry too much about your little one holding their head up. Their head will probably still be wobbly for another few weeks while their neck muscles continue to develop during tummy time, but you might notice that they're trying harder to move it around and hold it up for longer!
Top tip: To help test out how your little one feels about lifting their head up, try lying down facing them during tummy time, and say their name in your playtime tone of voice. As your little one starts to recognise familiar voices, they might try lifting their head to see you if they're ready!With all of your little one's growth they need a lot of milk to fuel it! Until they reach the six-month mark, breast milk is all your baby needs and this will provide them with all of the goodness and nutrients they need to thrive and grow.
By this point, your milk supply should be well-established. Ensure you stay hydrated and eat a nutritious diet to support milk production. Make sure both you and your baby are taking Vitamin D supplements.
If you're exclusively breastfeeding you should expect to nurse around 6 to 10 times in 24 hours by month two, but it can be as many as 20! In bottle terms, this tends to be an average of 720ml to 960ml of milk daily. But all babies are different and it's impossible to pinpoint exactly how often your little one will get hungry. Try not to obsess over volume or think your baby is not getting enough when they constantly want to feed. If they always seem hungry they are likely going through a growth spurt or are trying to regulate your milk. Breast milk production works on a supply-and-demand basis so the more your baby breastfeeds the more milk your body will produce.
Around six weeks old is typically their first growth spurt. During these periods your little one may seem hungrier and want to breastfeed more frequently. As mentioned above, this cluster feeding is entirely normal and helps stimulate your milk supply to meet its growing needs! Here’s more on boosting your milk supply.
At this stage most babies typically consume around 4 to 6 ounces (120 to 180 millilitres) of formula per feeding. However, it's important to note that babies may show signs of hunger or fullness and these cues should be considered. It's best to feed the baby when they display hunger signs, such as rooting, clenching and sucking on their fists, or making sucking sounds.
Remember that every baby is unique and their feeding needs may vary. Their nappy output is usually a good indicator of whether your baby is getting enough milk. Regular wet nappies, clear or pale urine and steady weight gain indicate this.
Sleep patterns for babies in the second month play a crucial role in their growth and development. During this month you can expect their baby to stay awake longer and be more responsive to their environment.
While babies are becoming more alert and interactive during the day, they still need around 15 hours of sleep daily. This will consist of 60-90 minute wake windows and 5-6 hours of daytime sleep spread across 4-5 naps. However it's important to note that sleep patterns can vary widely among babies. Some may wake up for feeds or nappy changes once at night, while others may sleep longer.
It's normal for babies at this stage to have a longer stretch of sleep at the beginning of the night, typically ranging from four to six hours. It's essential to manage expectations and understand that most babies are not yet sleeping through the night consistently.
Parents can establish a consistent bedtime routine to promote healthy sleep habits that signal the baby that it's time to wind down and prepare for sleep. This routine can include a warm bath, gentle massage, reading a bedtime story, or singing a lullaby. Creating a calm and soothing environment in the baby's sleep space in your bedroom, with dim lighting and a comfortable temperature, can also help facilitate better sleep.
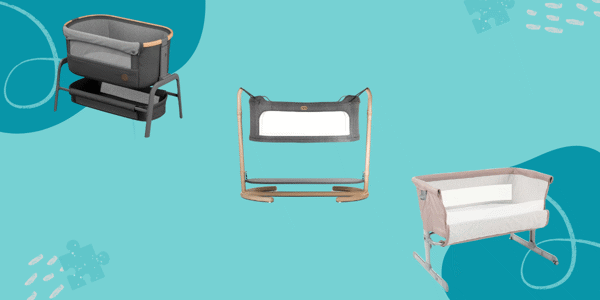
Make sure to respond to baby's needs at night. This includes feeding when hungry and changing nappies as necessary. Keeping the sleep environment safe by placing the baby on their back to sleep, removing loose blankets or pillows, and ensuring the crib or bassinet meets safety standards is crucial for reducing the risk of Sudden Infant Death Syndrome (SIDS).
Try to also prioritise your own sleep and well-being during this period. It can be challenging to adjust to the demands of a newborn but getting adequate rest whenever possible can help with overall physical and mental recovery. Sharing night feed responsibilities with a partner or asking for help from family and friends can provide support and allow mums to get the rest they need.
When parents struggle with their baby's sleep patterns or experience excessive sleep deprivation, seeking guidance from a healthcare professional or sleep expert is essential. They can provide personalised advice and support to address specific concerns and ensure the well-being of both you and your little one.
When your baby is around six weeks old you'll be asked to see your GP or health visitor for a check-up. All mums and babies have this six-week check. This is the time to mention anything you're concerned or worried about for your recovery or your little one's growth or development, no matter how big or small you think the issue may be.
The checks will be carried out in your local surgery or at home by your health visitor or GP. They help check everything is happening as it should be, ensuring you're healthy and any issues are picked up early. You can ask any questions and don't be afraid to talk about how you're feeling and doing mentally during this appointment. 'Baby blues' are expected; however, if those feelings have lasted over a few weeks, it is worth mentioning to your GP.
During the check on your little one, the doctor will do the following:
It's easy to forget about yourself during this check and make an appointment about your baby. If you have any questions about your recovery, whether physical or mental, ensure to raise these during the check-up. Whether it's regarding wound healing, weight, breast issues, energy, or your mental health, addressing any problems at this point can allow you to get the help you need and be signposted in the right direction, whether counselling, support groups, medication, or further medical care for any ongoing physical symptoms.
You will also discuss contraceptives and whether you wish to take them, get a prescription or book a follow-up appointment. Of course, if you are not ready to start having intercourse again, you can arrange another meeting to discuss contraception after birth, should you wish to take it in the future.
When your baby is eight weeks old they'll also be offered their first immunisations. This can be a scary thought when needles are involved, but it's vital that you attend your appointment and that your little one gets the protection they need from nasty infections, diseases and life-threatening illnesses.
During the first round of immunisations, your baby will get jabs to protect them against these infections and illnesses:
The second month postpartum is crucial for new mums as they recover physically from childbirth while caring for their newborns. Every mum's recovery looks different, from postpartum physical healing, including vaginal soreness, perineal healing, and caesarean incision care, to breast engorgement and managing postpartum bleeding; month two sees many women still recovering from the after effects of more complex deliveries.
Vaginal soreness is common following childbirth, especially if you had a vaginal delivery. This could be discomfort around the entrance, especially if you had an episiotomy or pain further into the canal, where forceps may have been used during delivery.
To alleviate discomfort try applying a cold compress or using over-the-counter pain relievers recommended by your healthcare provider. Good hygiene practices, such as using warm water to cleanse the area and patting it dry, can aid in keeping the perineum clean and promote healing. Additionally, sitting on a cushion or using a specialised doughnut-shaped pillow can relieve pressure on the perineal area.
If the pain/discomfort continues after a few more weeks/months, or you experience sharp pains or bleeding, consult your GP to ensure everything is healing.
For mums who underwent a caesarean section or had an episiotomy, proper care of the incision site is crucial in the first month. However it will still need to continue until fully healed. This can take up to 6-8 weeks. Keep the incision clean and dry, following your healthcare provider's instructions for cleansing and dressing. For an episiotomy, when urinating, it is best to use cool water to cleanse and pat dry rather than wiping, and try not to strain when pooing to avoid prolapse, rupture or dehiscence. This goes for c-sections too.
Following a caesarean, you'll still need to avoid lifting heavy objects and engage in light physical activity as advised. Supportive abdominal binders or underwear can offer gentle compression and reduce discomfort. If you notice any signs of infection, such as redness, swelling, or discharge, contact your healthcare provider promptly.
If breastfeeding, as your supply settles, your breasts can become swollen and tender due to increased milk supply. It is a common experience during the early postpartum period. Frequent breastfeeding, wearing a milk collector, or pumping with a breast pump can help relieve engorgement. Applying warm compresses or a warm shower before nursing can promote milk flow and prevent clogs in your milk ducts.
If you notice a hard wedge-like lump that is tender to touch, spot swelling and redness that is also hot to touch, feel a burning sensation all the time or while you feed, or have any discharge from the nipple that has streaks of blood, alongside any flu-like symptoms, call 111 or speak to your GP immediately, as it could be signs of mastitis. Breastfeeding women face this very common issue and can be treated with antibiotics to prevent it from developing into a more severe infection.
Continue to breastfeed your baby as usual, if not more often, offering the affected boob as much as possible to relieve any fullness and clear out the ducts. Massage your breast from duct to nipple whilst feeding to aid in this. You can also soothe breast pain with a warm or cold compress to assist milk flow, alongside lots of rest and liquids.
Postpartum bleeding, known as lochia, can be heavy in the first few days and gradually decrease. For the most part, it should have stopped by 6-8 weeks; however, some women experience this bleeding for longer. Your period may also have returned. Therefore it can sometimes be challenging to know if lochia has stopped or your period has begun. It's essential to use sanitary pads rather than tampons to avoid the risk of infection and any discomfort you may still be experiencing up there. Here’s more advice on managing postpartum bleeding.
The fluctuating hormones after giving birth can cause various physical symptoms, but one of the most common is vaginal dryness. This is caused by a lack of estrogen, which is responsible for increased blood flow and lubrication in your vagina. It can be responsible for hot flashes, night sweats, and a dry vagina. This can impact many new mums' ability to have sex again after having their little one. This dryness can make sexual intercourse feel painful, leading some new mums to avoid sex for this reason. This can last up to 6 months postpartum and could continue for those who breastfeed until they decide to stop.
There are no set rules about when to have sex again after giving birth, but listening to your body and mind and doing what feels right is essential. Even if you don't feel any physical pain it's totally normal not to think in the right headspace to have sex again at this point, and you shouldn't feel any pressure to do so. Using lubricant at this stage is still advisable.
When you do feel ready to begin having sex again after birth, it's important to remember that you can get pregnant as early as three weeks after birth, even if you're breastfeeding and your periods haven't started again. If you're exclusively breastfeeding, it's unlikely that you'll get your period back until around six months, though it may return earlier, though this doesn't always mean you aren't able to fall pregnant during this time. It's a good idea to start considering contraception during this time if you're ready to consider having sex again and feel physically and mentally comfortable doing so. You will have an opportunity to discuss contraception at your 6-week check or with your Health Visitor.
Mental health changes and emotional well-being are essential for the mother during this rather isolating, overwhelming time. It's crucial to prioritise self-care and seek support from healthcare providers, family, and friends to successfully navigate the postnatal period's challenges.
Many new mums experience postpartum mood disorders, such as postpartum depression and anxiety, during the first few months after giving birth. These conditions can significantly impact a mother's emotional well-being and affect her ability to care for herself and her baby. It's essential to be aware of the signs and symptoms of these conditions and seek help if needed. You can find much information on postpartum mental health here.
Postnatal depression is a common mood disorder characterised by persistent sadness, hopelessness, and a lack of interest or pleasure in your usual activities. Other symptoms may include changes in appetite and sleep patterns, irritability, fatigue, difficulty bonding with the baby, and thoughts of self-harm or harming the baby. Conversely, postpartum anxiety is characterised by excessive worry, restlessness, irritability, and difficulty sleeping.
Postnatal depression affects up to one in every five new mums, and it's nothing that you should ever be ashamed of. As the newborn bubble of the first few weeks wears off it's common to feel pressure to be happy in month two after having a baby when in reality you could be struggling.
If you're experiencing these symptoms, reaching out for support is essential. In the UK, resources are available to help mums with postpartum mental health concerns. A list of these can be found here. The first step is to speak with your healthcare provider, such as your GP or health visitor, about what you're going through. They can assess your symptoms, provide guidance, and refer you to appropriate mental health services.
In addition to professional help, several organisations and support groups in the UK focus on postpartum mental health. An organisation to consider is PANDAS Foundation, which specialises in supporting families experiencing perinatal mental health issues. They provide a helpline, online community and resources for both mums and partners.
Online resources can also be valuable sources of information and support. The NHS website offers comprehensive information on postpartum mental health, including symptoms, causes, and treatment options. Postpartum Support International (PSI) is an international organisation with a UK chapter that provides resources, helplines, and online support for mums and families affected by perinatal mental health issues.
Remember, seeking help is a sign of strength; you don't have to face postpartum mood disorders alone. With the proper support and treatment, you can navigate this challenging period and prioritise your mental well-being as you care for yourself and your baby. Other maternal mental health issues can include postpartum OCD, postpartum psychosis, birth trauma and PTSD following the delivery. To find out more about these, click here.
As you navigate the challenges of parenthood and get used to daily life with your little one throughout the second month, it's crucial to recognise the importance of getting out and about with your baby. Being a new mum comes with a wide range of emotions, and it's essential to have a support network during this time. Attending baby classes, support groups, and even just meeting up with loved ones provides an outlet for expressing your thoughts, concerns, and fears in a non-judgmental environment. It lets you receive emotional support, gain perspective from other mums and professionals, and help you remember that you're not alone in what you're going through.
During the second month postpartum, parents often experience significant changes and strains in their relationship as they adapt to the demands and challenges of caring for their newborn baby.
Sleep deprivation, round-the-clock responsibilities, and adjustments to their new roles can create tensions and conflicts in relationships with your partner, family and friends. However, parents can maintain a strong bond and open communication amidst the changes by recognising these challenges and taking proactive steps.
One common strain in the parents' relationship during this period is the division of labour and exhaustion. Both partners may feel overwhelmed and exhausted by the constant care required by the baby, leading to increased stress and potential conflicts. To overcome this, it is crucial for parents to communicate openly about their needs, share responsibilities, and offer support to each other. Breastfeeding as the primary care provider, in addition to the physical toll, can make the parental roles feel incredibly imbalanced for new mums.
Establishing a routine and finding ways to share parenting and household duties can help distribute the workload and alleviate some of the strain. Asking for help outside of your home, for example, from family or hiring home help, if you can afford it, could help relieve you of the stresses that come with the first few months of becoming a parent.
The information on the Your Baby Club website is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always discuss any health concerns with a qualified healthcare provider and carefully review all guidance that comes with any medications or supplements before taking.